Common benign womb growths with a rare possibility of causing malignancy.
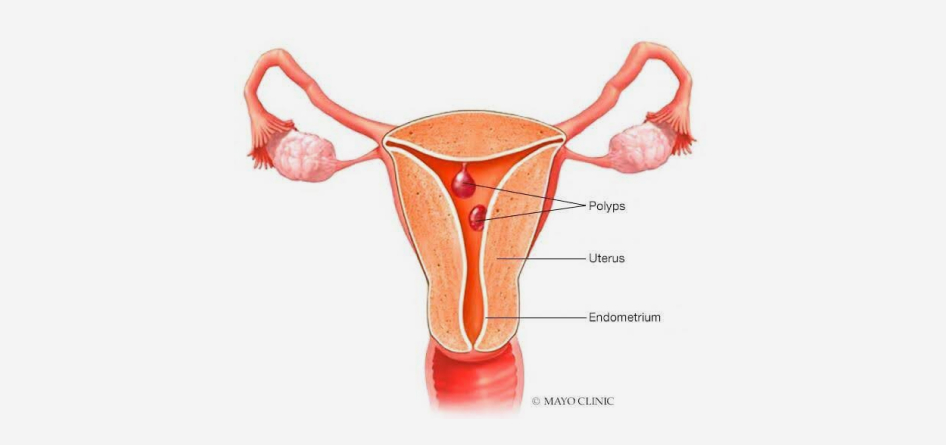
Endometrial polyps are benign growths of the inner covering layer of the womb that can vary in size (0.5-5 cm) and number (solitary or multiple). They are frequent in women aged 40-50.
There are three types of endometrial polyps. Functional polyps are more common in premenopausal women and grow along with the tissue. Atrophic polyps, which seem shrunk, are more common in postmenopausal women. Adenomatous polyps look regular, but contain smooth muscle tissue. They are rare but may be pre-cancerous, with the risk increasing with growth size (>1.5 cm) and carrier age (postmenopause).
A higher risk of developing endometrial polyps is associated with age and factors like obesity, hormonal influence, tamoxifen use (for breast cancer patients), genetic predisposition, hypertension, and diabetes. Polyps may recur within 1-2 years after removal.
Endometrial polyps are often asymptomatic (especially smaller ones), but when they have symptoms, they mostly have to do with bleeding. More rarely, polyps may interfere with the implantation of a fertilized egg, impairing fertility procedures. Usual symptoms include:
Abnormal uterine bleeding
Bleeding between cycles
Heavy menstrual bleeding
Bleeding after menopause
If you experience severe symptoms, please see a specialist as soon as possible.
Endometrial polyps are diagnosed through a step-by-step approach. Initial screenings include a transvaginal ultrasound and the more sensitive saline infusion sonography. However, hysteroscopy is the safest method for both identifying and treating polyps.
Removal by a minimally invasive hysteroscopic surgery is recommended when endometrial polyps are symptomatic. When there is a high risk of malignancy, such as in postmenopausal symptomatic women, the removed tissue is sent for a biopsy to rule out the small possibility of cancer.